Introduction
Organ transplantation has revolutionized the field of medicine, offering hope and a second chance at life to countless individuals suffering from organ failure. However, the demand for organs far exceeds the supply, leading to lengthy waiting lists and tragic outcomes for many patients. Cryogenic preservation of organs has emerged as a groundbreaking solution to this crisis, promising to extend the viability of donated organs and enhance the success of transplant surgeries. In this article, we will explore the science behind cryogenic preservation, its potential benefits, challenges, and ethical considerations, as well as its promising future in transplant medicine.
Understanding Cryogenic Preservation
Cryogenic preservation, also known as cryopreservation, is a technique that involves cooling biological materials, such as organs, tissues, or cells, to extremely low temperatures, typically below -130°C (-202°F). At these ultra-low temperatures, biochemical reactions virtually come to a halt, preventing cellular damage and degradation. People often use this preservation method in various fields, including biobanking, fertility preservation, and more recently, organ transplantation.
The Cryopreservation Process
Cryogenic preservation of organs is a complex and meticulous process that requires careful handling and precise temperature control. Here is an overview of the key steps involved:
- Organ Procurement: The process begins with the retrieval of the donor organ. Once we identify a suitable donor, we harvest and prepare the organ for cryopreservation.
- Organ Perfusion: To remove blood and minimize ice formation, typically perfuse the organ with a specialized cryoprotectant solution. This solution replaces water in the cells, reducing the risk of ice crystal formation that could damage cell structures.
- Controlled Cooling: We gradually cool the organ to the desired cryogenic temperature using controlled-rate cooling devices. This step prevents the formation of ice crystals, which can be harmful to cells.
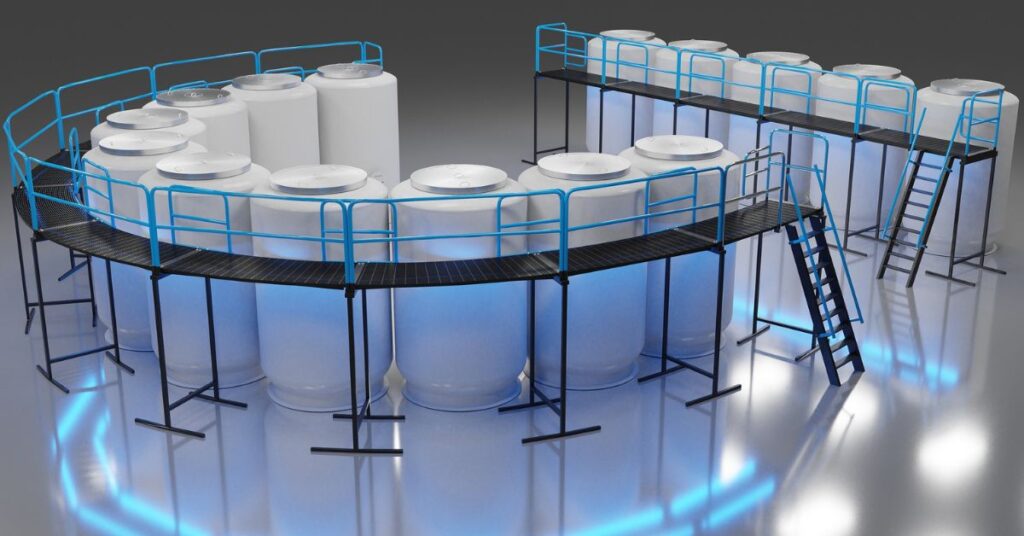
- Storage: Once the organ reaches the target temperature (usually around -196°C or -321°F), it moves to a storage container filled with liquid nitrogen, and it can remain there indefinitely. The low temperatures effectively stop all metabolic processes, preserving the organ until someone needs it.
- Thawing and Transplantation: When a suitable recipient becomes available, specialists carefully thaw the organ and get it ready for transplantation. They gradually eliminate the cryoprotectant and warm the organ to physiological temperatures before transplanting it.
Benefits of Cryogenic Preservation
- Prolonged Viability: Cryogenic preservation extends the shelf life of organs significantly. Conventional organ preservation techniques, such as cold storage, can maintain organs for several hours, but cryopreserved organs can remain viable for years, if not decades.
- Enhanced Organ Matching: Cryopreservation allows for better matching of donor organs to recipients. Cryopreserving and storing organs until a suitable recipient is found reduces the pressure to find a perfect match within a limited timeframe.
- Reduction in Organ Shortage: By increasing the availability of viable organs for transplantation, cryogenic preservation has the potential to address the severe shortage of donor organs, potentially saving countless lives.
Challenges and Limitations
Despite its promise, cryogenic preservation of organs faces several challenges and limitations:
- Cryoprotectant Toxicity: The use of cryoprotectants can be toxic to cells and tissues. Finding the right balance between protecting cells from ice damage and avoiding cryoprotectant-induced toxicity remains a challenge.
- Ischemia-Reperfusion Injury: The process of thawing and transplanting cryopreserved organs can trigger ischemia-reperfusion injury, where the restored blood flow can damage tissue. Strategies to mitigate this risk are still under development.
- Quality Control: Maintaining the quality and viability of cryopreserved organs over extended periods requires meticulous monitoring and quality control. Ensuring that the organs remain safe and effective for transplantation is an ongoing challenge.
- Ethical Considerations: There are ethical concerns surrounding the long-term storage of organs and the potential commodification of organ banks. Ensuring equitable access to cryopreserved organs while avoiding exploitation is a critical issue.
The Ethical Dimensions
Cryogenic preservation of organs presents ethical considerations that must be addressed as this technology advances:
- Resource Allocation: The allocation of cryopreserved organs raises questions about fairness and equity. How should these precious resources be distributed to ensure equitable access for all patients in need?
- Informed Consent: Donors and recipients must provide informed consent for cryopreservation, with a clear understanding of the potential risks and benefits. Ethical guidelines for this process must be established and upheld.
- Long-term Storage: The indefinite storage of organs may raise concerns about the ethical implications of keeping deceased individuals in a state of suspended animation. Striking the right balance between respecting the deceased and saving lives is a complex ethical challenge.
- Commercialization: There is a risk that cryogenic organ preservation could become a profitable industry. Ensuring that profit motives do not compromise the ethical principles of organ donation and transplantation is crucial.
The Future of Cryogenic Organ Preservation
Despite the challenges and ethical concerns, the future of cryogenic organ preservation is bright. Ongoing research and advancements in the field are addressing many of the current limitations. Here are some exciting developments to look forward to:
- Improved Cryoprotectants: Researchers are working on developing less toxic cryoprotectant solutions that will better protect cells during the preservation process.
- Enhanced Thawing Techniques: Innovations in organ thawing techniques aim to minimize ischemia-reperfusion injury and improve post-transplant outcomes.
- Regulatory Guidelines: Ethical guidelines and regulatory frameworks are being established to ensure the responsible use of cryopreserved organs and protect the rights and dignity of donors and recipients.
- Artificial Organs: In the future, scientists hope to develop artificial organs that can be cryopreserved and used as replacements, reducing the reliance on human organ donors.
Cryogenic preservation of organs holds immense promise in the field of transplant medicine. By extending the viability of organs and addressing the chronic shortage of donor organs, this technology has the potential to save countless lives. However, it also brings forth complex ethical considerations that demand careful consideration and regulation. As research continues and technological advancements progress, cryogenic organ preservation may emerge as a pivotal element in the future of organ transplantation, providing hope to patients requiring life-saving procedures.
Now Read This – Insect Farming : A Sustainable Solution for the Future of Food


Leave a comment